Luteal Phase Defect
Knowing one’s healthy menstrual cycle hormones can help identify where the problem is in any sort of dysfunction. A luteal phase defect is when there is a disruption in a woman’s monthly menstrual cycle. The luteal phase is one phase of the cycle occurring after ovulation and before the bleeding (period) begins. It is during the luteal phase that the lining of the uterus normally becomes thicker to prepare for a possible pregnancy. A defect would not allow for the lining to grow adequately making it difficult to get pregnant or maintain a pregnancy. Another common name is an abnormality in the endometrial development. These mechanisms may cause an inadequate endometrial response to hormonal stimulation during the luteal phase:
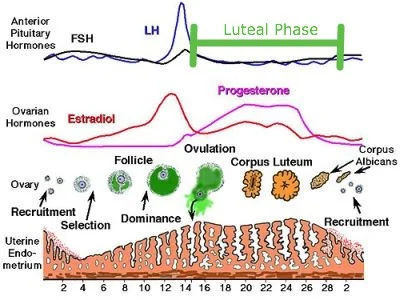
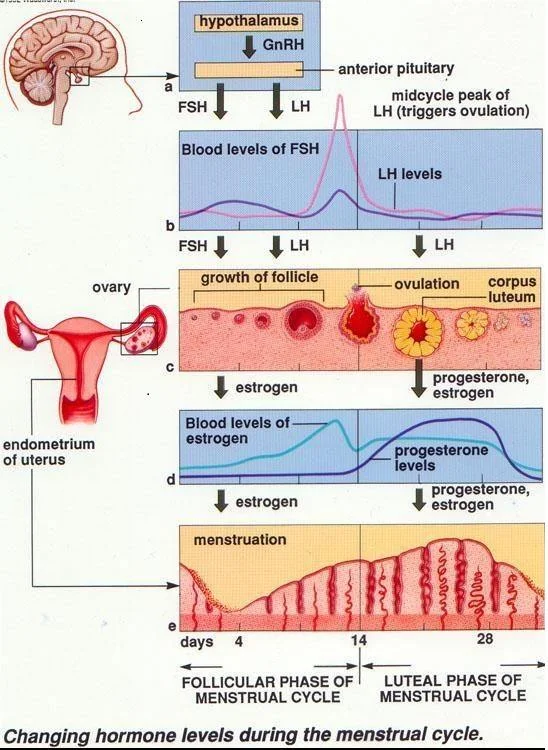
Abnormal follicular development –from inadequate follicle-stimulating hormone (FSH) and luteinizing hormone (LH) secretion from the anterior pituitary gland. FSH stimulates the granulosa cells of the developing follicle to produce estradiol from the conversion of its substrate androstenedione. A decrease in FSH release results in reduced granulosa cell growth and lower estradiol levels. Because the corpus luteum is not a de novo structure but is a direct result of the follicle, it shows the effects of abnormal folliculogenesis with decreased progesterone production.
Abnormal luteinization –can cause a decrease in androstenedione from the theca cells. Less substrate results in a decrease in estradiol and, subsequently, lower progesterone levels. Additionally, a suboptimal LH surge at ovulation causes deficient progesterone because of inadequate luteinization of the granulosa cells.
Uterine abnormalities –cause changes in vascularization of the endometrium despite normal progesterone levels. Myomas, uterine septa, and endometritis are responsible for poor secretory changes in the endometrium.
Hypocholesterolemia –substrate responsible for initiation of the steroid pathway. A deficiency results in low-to-absent progesterone production and a luteal phase defect.
The patient will present with a menstrual cycle of less than 26 days or a luteal phase of less than 11 days by basal body temperatures. Because during a normal cycle, a woman’s internal temperature rises due to the hormonal changes between LH and progesterone. The defect may also arise if the ovaries do not release enough progesterone or the lining of the uterus does not respond to progesterone. Symptoms include more frequent periods, miscarriages, difficulty getting pregnant and spotting between periods.
Health conditions which may cause luteal phase defect:
Anorexia,
Endometriosis,
Extreme amounts of exercise,
Hyperprolactinemia (excess of a hormone that’s responsible for milk production in breasts),
Obesity,
Polycystic ovarian syndrome,
Thyroid disorders.
To diagnose luteal phase defect, the physician will do a blood test for:
Follicle-stimulating hormone (FSH),
Luteinizing hormone (LH),
Pregnancy test,
And progesterone levels.
Also, some physicians may do a biopsy for confirmatory results, but a pregnancy test has to be done beforehand. A new marker has been identified to determine if the lining of the uterus is ready for pregnancy, the beta-3 integrin.
Treatments for the defect include:
Clomid(clomiphene citrate) stimulates your ovaries to make more follicles, which release eggs,
Human chorionic gonadotropin(hCG) may help induce ovulation and produce more progesterone,
Progesterone injections, pills, or suppositories may be used after ovulation to help the lining grow.
Those who live in Denver may visit the Denver Holistic Center for more information about the luteal phase defect and treatment options that may be suitable for their case.
Figure 1 – Phases of the menstrual cycle.
Figure 2 – Normal menstrual cycle and hormones.
Luteal phase is an important part of the normal menstrual cycle of each and every woman, a defect is easily detected and may be treated, so do not hesitate to meet with your OB to discuss treatment options.